Health Care System — Entity Diagram
Announcing Nightingale
Software capabilities to improve health care.
Hello World.
February 1, 2024
Our manifesto:
Health care delivery today is primarily an information problem. Highly trained doctors and nurses take in data points and signals about patients from various primary and secondary sources, and perform complex decision-making that results in diagnoses, treatment decisions and care plans.
It is also a federated system by design, with a vast range of separately governed and operated service providers, suppliers, and insurers — not just across patients, but even with respect to a single patient. Of course this is true in privatized health care systems like the U.S., but surprisingly also in public ones like the U.K. (albeit to a lesser degree).
The diagram below shows the entity categories that make up the delivery system, with each entity having their own localized patient (consumer) information system and data model, frequently with little normalization or standardization even internally.
To be sure, the distributed nature of the delivery system has governance, operational and competitive benefits, but from an information systems point of view it has led us to a state of a lot of untapped potential energy.
That's why we founded Nightingale. Advances in the last several decades in compute, data models, connectivity (both generally, and specifically to health care) — as well as necessary progression in health care payment models in parallel — place us at a takeoff juncture of immense capability acceleration. The infrastructure, combined with compelling value creation, capture and reinvestment feedback loops, now exist to overcome previous architectural and implementation problems.
Fundamentally, at Nightingale's base layer we have architected a "superchart" — a high fidelity, comprehensive patient data record — which serves as the backbone for (a) simply rendering a more complete and usable pane of glass for providers and staff members to reference directly, and (b) ultimately delivering advanced intelligence to vastly augment provider and staff review and care delivery processes, and close blind spots.
With our private preview rollout in 2024, Nightingale represents the culmination of our founding team's prior years of research and development in the areas of patient data retrieval, normalization and reconciliation across service providers, suppliers and insurers, combined with a deep operational awareness of health care professional and supporting personnel workflows and patient engagement patterns. A lot of this foundational development might typically be thought of as "boring plumbing" work, but we believe it is a prerequisite for the basic and advanced intelligence use cases that are now coming to fruition. In our view, the information problem (and opportunity) in health care starts with the quality and robustness of the patient data model and record.
An initial focus on health care's "super users'' :
Equally important to the what is the who. To start, we our rolling out the platform to support senior care with physician organizations in the United States. In many ways, these are health care's "super users'' — not just locally but globally. Across countries, the U.S. is far and away the #1 utilizer of health care resources — it's more than triple the runner-up (Germany). And within the U.S. (and really any country for that matter), seniors are by far the largest consumers of health care: just as a car with more miles on it needs more maintenance and time in the shop, our bodies require more upkeep, management and medical services as we age.
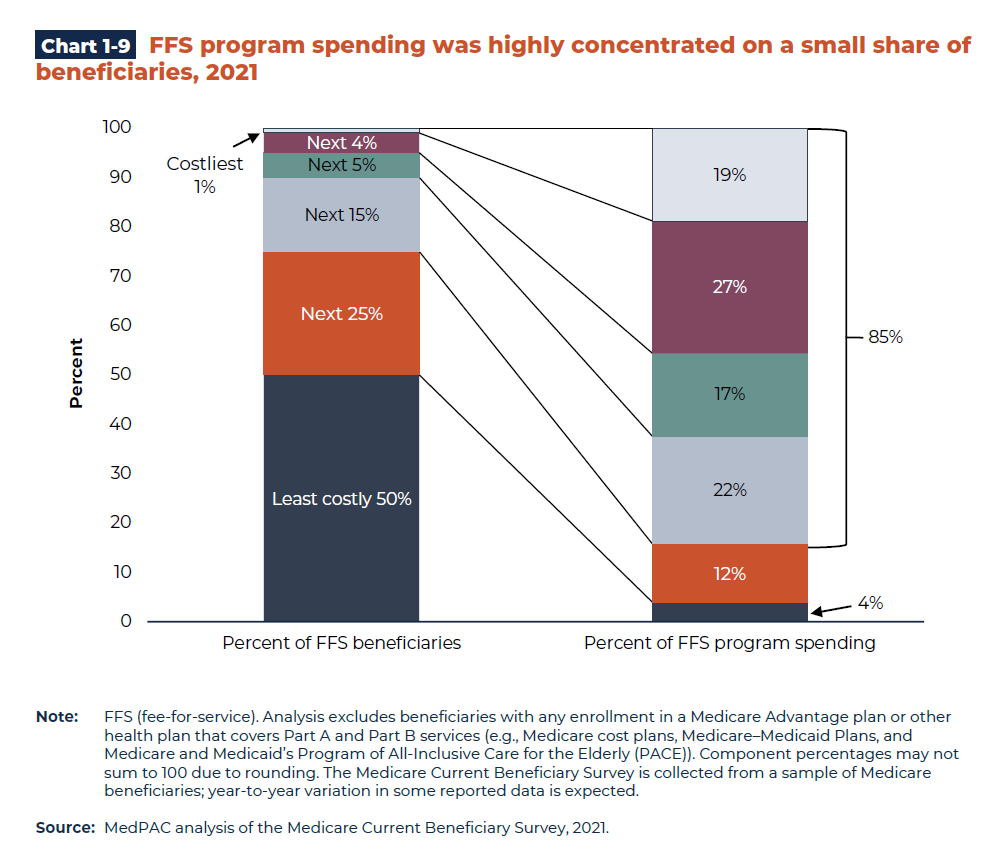
Telescoping further, within the Medicare population in the U.S. every year, 5% of members result in 44% of all health care service utilization (see chart below), largely as a result of a high incidence of hospitalization and other acute and reactive disease and symptom management interventions. This side of the spectrum might be thought of as the "super super users," and these are the ones with the greatest immediate opportunity for improvement and impact.
An aligned, outcome-driven business model:
Our go-to-market business model is centered on partnering exclusively with physician networks in a Medicare total-cost-of-care "risk model": in this model, a physician organization (made up of primary care and/or specialist doctors) enters into an agreement with Medicare whereby instead of getting paid strictly as a function of the number of visits or services they provide (called "fee-for-service"), they instead are given a fixed budget (called "capitation") to cover all of the patient's services across all providers and suppliers.
We have selected this model because it aligns our care improvement mission with our financial model. In this structure, profit is generated only if the organization delivers high-quality preventive care and disease management and reduces emergency and acute spiraling events for their patients, since these are the "big ticket items" that drive a majority of the expense (especially, again, for the 5% of patients who are super users).
In the long run, "follow the money" determines where companies innovate and invest (see Google with AdWords and Facebook with its marketing engine), and so the selection of our go-to-market business model was equally as important as what and how we build. We are currently in private preview with our first launch partner, and plan to begin accepting additional physician organizations and networks in early 2025.
Additional Principles:
- Human in the Loop. Even in low-risk situations, all of our non-deterministic, advanced intelligence outputs use a human review-and-relay approach to integrating with the medical team.
- EMR Agnostic. Without rebuilding the entire delivery system from scratch, electronic medical records will remain varied and fragmented. We believe our solutions should function irrespective of existing EMR infrastructure and assets that providers have in place.
- 10x not 1.2x. While we are selective in what problems we choose to tackle in our roadmap, when we decide to solve a use case we have a bar of achieving a 10x improvement vs status quo solutions (in either capability or efficiency), not a 20% bar as is commonly used in industry.
The road ahead
We are motivated by the progress we have made so far, and we are equally humbled by the roadmap ahead and are always on the lookout for the brightest minds. If you are interested in working on large information and engineering problems with major human impact, reach out to us!


